SOM Researchers Study Ketamine in Depression
For years, scientists and doctors have known that ketamine can treat depression very rapidly, often working within hours, compared to weeks or months for widely used antidepressants. However, the drug, which is approved as an anesthetic, has major side effects – it is linked to hallucinations and dissociation - a sense of being outside your own body – and for these reasons is abused as a club drug. Not surprisingly, this limits its use in the treatment of depression.
A solution may be at hand. Preclinical research at the University of Maryland School of Medicine has identified a metabolite of ketamine that quickly reverses depression in mice, but without ketamine's side effects. The study was published today in the journal Nature.
“This is potentially a major breakthrough,” said the study's senior author, Todd Gould, MD, associate professor of psychiatry at the School of Medicine. “It could allow depressed patients to get the rapid benefits of ketamine, while at the same time avoiding the risks.”
Most people with depression take medications that increase levels of the neurochemicals serotonin or norepinephrine in the brain. The most common of these drugs, such as Prozac and Lexapro, are selective serotonin reuptake inhibitors, or SSRIs. However, SSRIs are effective in only half of patients with depression, and even when these drugs work, they typically take between three and eight weeks to relieve symptoms. Ketamine, which does not work via serotonin or norepinephrine, can lift depression much more quickly, within hours after administration.
The work was a collaboration among scientists at the School of Medicine, the National Institutes of Health's (NIH) National Institute of Mental Health (NIMH), the National Center for Advancing Translational Sciences, the National Institute on Aging, and the University of North Carolina.
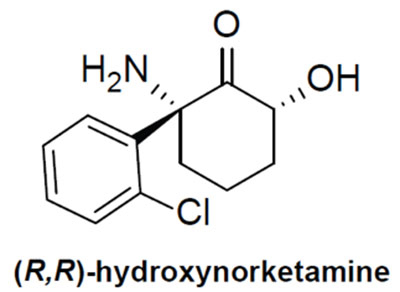
The compound hydroxynorketamine.
“For years, we have been searching for ways to treat depression faster and more effectively,” said co-author Scott Thompson, PhD, professor and chair of the Department of Physiology at the School of Medicine, who has spent more than a decade studying glutamate and depression. “These results open up exciting new vistas for the first new generation of antidepressant compounds in the last 30 years.”
Using mice, the researchers tested the effects of several ketamine metabolites, chemicals produced by the breakdown of ketamine. They eventually focused on one called hydroxynorketamine, a compound that had been thought to have no psychoactive effects. In mice, blocking the transformation of ketamine to hydroxynorketamine prevented ketamine's antidepressant actions. Hydroxynorketamine itself also showed antidepressant effects, and none of ketamine's side effects.
“This discovery fundamentally changes our understanding of how this rapid antidepressant mechanism works, and holds promise for development of more robust and safer treatments," said Carlos Zarate, MD, of NIMH, a study co-author and a pioneer of research using ketamine to treat depression. "By using a team approach, researchers were able to reverse-engineer ketamine from the clinic to the lab to pinpoint what makes it so unique.”
The anesthetic and dissociative actions of ketamine are due to the fact that it blocks a particular glutamate receptor, the NMDA glutamate receptor. Researchers had assumed that ketamine acts as an antidepressant via the same mechanism. This appears not to be true, however, because hydroxynorketamine does not inhibit the NMDA receptor. Instead, hydroxynorketamine seems to activate another type of glutamate receptor, the AMPA receptor. Gould says that hydroxynorketamine likely works on depression via these AMPA receptors, either directly or indirectly.
Gould and his colleagues at the NIH are already planning to begin testing hydroxynorketamine for its safety in humans. But he points out that the compound has, in effect, already been in humans for years as a metabolite following ketamine administration. "This gives us confidence it will be safe," said Gould.



